As pet parents, we would do anything to keep our furry friends happy and healthy. We go the extra mile (or extra thousand miles) to help them when they are in distress. One way to look out for your pet’s well-being is by incorporating Reiki healing into their well-rounded care routine.
Continue reading to learn more about Reiki healing and how it may help soothe your pet.
What Is Reiki Healing?
Reiki healing is an ancient form of therapy that can be used to soothe physical, mental, and emotional pain. Reiki practitioners attempt to deliver energy to the body through a technique called palm healing. Palm healing is supposed to balance energy to promote relaxation and reduce some physical and emotional pain.
Some humans swear by Reiki healing, but can it help dogs?
What Are the Potential Benefits of Reiki for Dogs?
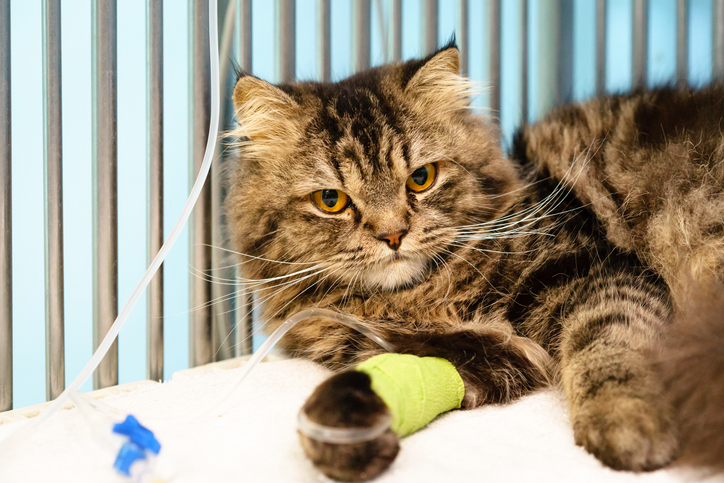
Dogs benefit from Reiki in similar ways to humans. It might help dogs adjust to situations that might otherwise be anxiety-inducing (such as going to a new place or meeting new animal friends). It may even assist in recovery after illness, injury, or surgery.
Here are a few ways your dog could benefit:
Stress Relief
One of the main overall benefits of Reiki for anxious animals is that it may relieve stress. Reiki is often associated with warm sensations that participants find particularly soothing.
When a Reiki practitioner creates a calm environment through meditation, then invites the dog to think about joining, the dog could gradually feel more peaceful and less anxious. This practice could be especially helpful for dogs in high-stress environments such as crowded shelters and homes with multiple people or pets.
Medical Care and Recovery
For dogs experiencing illness or recovering after surgery, Reiki may encourage the body to repair itself naturally while easing muscle tension. This practice could help pups decompress before receiving medical care as well.
Trauma and Behavioral Problems
Sometimes, Reiki supports dogs in animal shelters who are struggling with overstimulation, boredom, and unpredictability.
Reiki may help them overcome trauma from their past and resolve behavioral problems, possibly increasing their chances of successfully transitioning into a new home. While Reiki shouldn’t replace traditional behavioral training techniques, it can be a great addition to a trainer’s toolbelt of resources.
Grieving Process
If a dog is grieving a human or pet family member who has passed, Reiki could possibly provide a sense of peace while adjusting to life without their loved one.
End of Life Process
Reiki could help dogs who are about to pass feel tranquil before crossing the rainbow bridge.
Bonding
Reiki can allow you to connect with your dog and spend time with them in a way that benefits both of you. When you share that gentle, compassionate space with them, it might be easier for them to open up to you.
If you have brought home a new dog who is having trouble getting acclimated to an unfamiliar environment, this practice can encourage trust and a sense of belonging. Reiki might provide a healthy space to allow them to feel like themselves again.
How To Perform Reiki for Dogs
Now that you know what Reiki is and how it can help your dog, you might be wondering how to perform it. Let’s discuss some hand positions and give basic instructions so your dog might fully benefit from this practice.
Reiki is non-invasive. It only uses touch to transfer energy from you to your dog, and they do not feel any pain during the process. This makes it easy to perform anywhere, anytime.
Each position should be held for a few minutes to allow them the opportunity to begin to decompress. It is more effective to start at the top of your pup’s body, then move downwards throughout the session.
Hand Positions and Techniques
- Shoulders: Put your right hand on your dog’s left shoulder and your left hand on the right shoulder. You may need to modify the placement of your hands based on your dog’s position.
For instance, if your dog is on their side, place both hands on the side of their upward-facing side. If they are standing or sitting, place one hand on each of their shoulder blades from behind. This position, like all positions, should be held for several minutes (or as long as your dog is enjoying it).
- Midsection Area: Center both hands on the middle of your dog’s stomach if they are lying down. If they are standing or sitting, put your hands on both sides of the spine.
- Chest and Head: Place one hand on your dog’s chest and the other on their head between their ears.
- Chest and Back: Center one hand between your dog’s shoulder blades and the other on their chest.
- Lower Back: Put your hands side-by-side on your dog’s lower back, directly above the tail. When your dog is lying on their side, your hands can remain next to one another. For this technique, you should put one hand on each side of the spine when your pup is standing or sitting.
How To Create a Positive Atmosphere
Like in all manners of dog training, positive reinforcement and having a fun time is key.
It is important not to force dogs to participate in Reiki but simply hold space for them and invite them to join. This ensures they won’t feel anxious throughout the session and can take things at their own pace.
Over time, your dog could be more inclined to participate when they see that you continue to hold space in a gentle, supportive manner.
If your pup is asking a little shy, here are some ways to encourage them to get in on the fun:
Continue Holding Space
If your dog is uninterested at the beginning of the first session (or for the first few sessions), remember that it will take time for them to become accustomed to Reiki.
As you continue to create and hold a relaxed space, it will be easier for them to be open to the process. The purpose of Reiki is to transfer your own zen energy to your dog. If your energy is strained, your dog might not be receptive to it. You will see better results when your dog is slowly introduced to Reiki.
Let Your Dog Lead
Don’t try to control the session. Give your dog time to feel comfortable in the space and let them show you what feels right while you observe your pup’s reaction.
When your dog feels like they hold their fate in their own paws, it can help make the overall process go smoothly.
Be Patient
When practicing Reiki with dogs, results are hardly ever immediate. Some dogs may have more difficulty or react differently than others. With patience (or maybe a treat and tummy rub), dogs could be more receptive to Reiki as you continue.
Can Pet Parents Benefit From Giving Reiki?
We’ve talked about how your dog can benefit from this treatment, but what about the pet parent, aka you? You’ll be glad to know that Reiki is mutually beneficial even when it’s focused on your dog’s well-being.
Here are some ways Reiki could help you become a better companion to your best friend:
- Connection: Reiki creates a steady environment that both you and your dog can share, providing an opportunity for you to connect on a deeper level. You might notice that using Reiki helps you better understand your dog’s behavior and moods.
- Relaxation: Reiki is meant to relieve any tension or stress your dog may be feeling. By holding this calm space for them, you can start to feel more serene along with them.
- Easily Accessible: Reiki can be done anywhere and doesn’t require special tools or equipment. Just head to your dog’s favorite space to chill and get ready to unwind.
Help From Animal Reiki Practitioners
If you prefer an Animal Reiki Practitioner to work with your pup, the prices tend to vary based on the number of sessions and the length of each session. Some Animal Reiki Practitioners will perform at-home sessions, which could cost more than regular sessions.
Virtual Reiki sessions are also an option, which some dogs might respond better to (depending on their demeanor and comfort level around strangers in their space). Online courses and tutorials that can help you learn Reiki independently may be less expensive than professional sessions. Plus, you learn a new skill and spend some quality time with your favorite fluffy friend!
Is Reiki Right for My Pet?
Reiki could be combined with traditional veterinary medicine practices as well as other forms of behavioral training, preventative care, and diet and exercise. If you’re unsure about which practices are best suited to your furry friend, you can reach out to AskVet.
AskVet’s Certified Pet Lifestyle Experts™ are here to be the best friend of man’s best friend. They are here to advise loving pet parents on anything and everything. Connect to the AskVet app for just $9.99 a month to put all four paws forward.
Sources:
All About Reiki: How This Type of Energy Healing Works, and Its Health Benefits | Everyday Health
Reiki Healing for Pets: Is It Possible? | American Kennel Club